Crohn’s Disease: A natural approach
I had the pleasure of interviewing Tristan Biesecker, of Biesecker Laboratories in Washington State. Tristan, along with his father and a talented crew of researches, are chipping away at the complex puzzle of Crohn’s and other inflammtory bowel conditions (IBD). Tristan also has a strong interest in effective, science based complementary approaches to IBD and has shared some of his finding, insight and experience with us. Sit back, you are in for a treat!
Question 1: Can you explain what is different about the intestines of those with Crohn?s disease?
There are various components that must function properly in the gastrointestinal
tract in order for the intestine to remain healthy. To keep things simple, I will stick
with what we believe are the most important. First, the mucus barrier. Throughout
the GI tract, there is a mucus barrier that coats the lining of the intestine. It serves
many purposes, many of which we still don’t fully understand. However, there are a
few that we have pretty well de?ned. First, it acts as a barrier between the bacteria
present in the lumen and the underlying tissue. Second, it can also serve as a
location for good bacteria (or normal microbiota) to live and thrive. The complex
structure and internal functioning mechanisms of the mucus barrier are beyond the
scope of this response, but normally the good microbiota inhabit the mucus lining
without invoking an immune response. In a Crohn’s patient, it appears the mucus
barrier is either gone or degraded to such a degree that it can’t properly function. We
don’t fully understand why the mucus barrier is destroyed, but once it is, it makes
sense that your body would produce an immune response: the bacteria are then
able to penetrate the tissue, at which point the body doesn’t care if the bacteria is
“good”, it just knows that a foreign invader is present in an area that it shouldn’t be.
We suspect that environmental factors play a signi?cant role in the degradation of
the mucus barrier. Particularly, we believe that surfactants, emulsi?ers, and other
food additives are the likely culprits. For instance, dexstran sodium sulfate (which is
in lots of cleaning products like dishwasher detergent) and carrageenan (a very
common thickening agent) have been proven to cause colitis a in mice. In our
model, the constant ingestion of these surfactants and emulsi?ers in part (perhaps a
great part) prevents the body from properly restoring the mucus barrier. We also
suspect that there is a bacterial component, such as sulfur-reducing bacteria (SRB).
These SRBs feed on the sulfur groups that are vital components of the mucus
barrier. Once these sulfur groups are destroyed, the integrity of the mucus barrier is
compromised. We are working to gather more evidence to support this observation.
Question 2: How is Crohn?s disease different from other inflammatory bowel conditions?
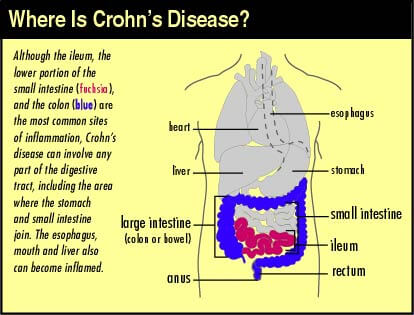
The two primary in?ammatory bowel diseases are ulcerative colitis and Crohn’s
disease. On a clinical level (looking through an endoscope) they are often confused;
however, Crohn’s disease does usually have distinct microscopic differences from
ulcerative colitis, such as the presence of granulomas. Moreover, in rarer cases,
Crohn?s can have systemic problems ranging from skin lesions to herpes-like sores
in the mouth. On the other hand, ulcerative colitis only affects the colon (and
perhaps a portion of the ileum) in almost all cases. Unfortunately, the differences
etiologically and pathogenically between Crohn?s disease and ulcerative colitis have
not been explored thoroughly enough. We recognize some microscopic differences, but signi?cant etiological differences have not been fully de?ned.
Question 3: We know that immunosuppressive therapy is the primary ? and often only ? choice of treatment for Crohn?s disease and other inflammatory bowel disease. What are the advantages and disadvantages of this approach?
Twenty (even ten) years ago, the medical community believed that Crohn?s was an
autoimmune disease; in other words, the body?s immune system is dysfunctional
and attacks its own tissue. Thus, the application of immunosuppressants, which
remains the primary treatment method in the United States. Currently, the research
community believes that there is a ?dysregulation? of the immune system, resulting in a chronic and dif?cult-to-control immune response. They also believe there is some
complex interplay between the immune system and enteric bacteria, but there is no
clear consensus on the nature of that interaction. Some groups believe it?s a matter
of ?immune tolerance?. In this scenario, the body somehow loses tolerance of the
microbiotia, or i.e., decides to eradicate good bacteria along with the bad, and
therefore the body produces an extensive immune response to accomplish said
goal. Other groups are looking into the degradation of the mucus barrier and how
that plays a role pathogenically. Regardless of the etiological nature of Crohn?s
disease or ulcerative colitis, immunosuppressants have been proven to help
because they work to reduce the overall immune response. Essentially, they reduce
the ?ow of gasoline to the ?re. However, this approach does not target the
underlying cause(s) of these diseases. Thus, it?s ef?cacy leaves much to be desired.
Moreover, some of the side effects of this treatment protocol are more serious than
what it?s treating. By taking immunosuppressants, you risk developing other
conditions such as lupus and life-threatening diseases such as malignant lymphoma.
When considering this treatment option, the situational parameters need to be
measured carefully. Have I tried all alternative treatments? Am I at a stage where
alternative treatments aren?t options? Would I rather suffer through Crohn?s or try
immunosuppressants and risk death? And many more.
Question 4: Through your work, you have discovered that there are additional, effective ways of treating Crohn?s that don?t necessarily include the use of steroids. Would you explain that to us?
Through our research we have come across a treatment protocol that more
effectively targets what we believe are the primary issues in Crohn?s disease. The
protocol that I follow consists primarily of antibiotics and probiotics. The current (I
emphasize ?current? because our notions are constantly being adjusted) idea is that
the antibiotics target the bacteria your body is having an immune response to ?
which in turn mitigates the immune response because there are fewer bacteria to
deal with ? and also targets potential bacterial culprits that could have a roll in the
etiology of Crohn?s (like sulfur-reducing bacteria). Probiotics are used to replace the
good bacteria necessary for healthy gut function. I also take supplements that have
been shown to aid in reinforcing the mucus barrier. In short, this protocol attempts to
?x the actual problems in Crohn?s disease, whereas only using immunosuppressants
and steroids does not. However, this treatment protocol is no cure. Although it does
seem quite effective in a decent percent of patients, people do recur on this
treatment. We are still gathering statistical data on the overall ef?cacy of this
protocol (this is a slow task as most physicians won?t prescribe this protocol). It?s not
the ultimate solution, but we think it?s a step in the right direction.
Question 5: What lifestyle suggestions do you have to offer people with inflammatory bowel disease? Is there anything that they can do in their day-to-day life to feel better?
Although I believe the cure for IBD lies with medical treatments, actions can be
taken in your daily routine to improve your quality of life. Our research has shown
that many bad chemicals are present in our foods and drinks. Large companies have
introduced these additives to preserve shelf-life, enhance colors, alter odors,
conserve consistency, and more. Now these additives have become the norm for
even small companies. Unfortunately, it?s only now being discovered that some of
these additives can have a signi?cant effect on your health. All of the gums in
products are there to preserve the consistency (keep it smooth) and prevent
separation of the various ingredients. We often refer to these as emulsi?ers or
thickeners. Emulsi?ers are in almost everything these days because they are a
cheap and effective way to create products that last and have a homogenized look. A perfect example is a typical chocolate candy bar; if you look at the ingredients list
you?ll ?nd soy lecithin, a common emulsi?er used to homogenize the milk and
chocolate mixture. Then, there are the chemicals we?ve added to cleaning products
to make them ?more effective?. And in some cases, these chemicals really do
enhance the effectiveness of the product, but they are ultimately unnecessary. For
instance, dexstran sodium sulfate (DSS) is a common chemical in soap and
toothpaste products. DSS makes it so you don?t need your plates to be wiped clean
before you put them in the dishwasher ? in other words, you can leave you dishes
dirty before you put them in the dishwasher, and after the run is done, they will come
out ?clean?. But they aren?t really clean because they usually have DSS residue left
on them (remember DSS has been proven to cause colitis in mice models).
Question 6: Tell us about the future for Crohn?s disease research and management.
It is our hope that more physicians will begin to recommend a treatment protocol that
consists of antibiotics and probiotics before more toxic treatments (such as
immunosuppressants) are used. However, this probably won?t occur until we gather
more evidence to support the bacterial model of Crohn?s. Moreover, the medical
community is very slow to offer other treatment options, unless of course a cure has
been found. What does this mean for management? Unfortunately, it looks like
immunosuppressants and steroids will be the primary forms of treatment for quite a
while. However, in the research world, the bacterial model is gaining more and more
traction. By our estimation, with the amount of research now on IBD, we hope that
Crohn?s will be de?ned (i.e., we know its etiology and pathogenesis precisely) within
the next ?ve years. Once that understanding is acquired, a totally effective treatment
or cure should be synthesized within a few years. To conclude, we hope that Crohn’s
will be solved within 10 years; everyone just needs to hold on. In the meantime, we
have created a company (Dr. Biesecker’s) that sells products designed for Crohn’s
patients and anyone else who wants to live a healthier lifestyle. We have designed
these products with our theories in mind; thus, they are devoid of the potentially
harmful compounds I mentioned above. It will be coming online in December or
January.
Thank you so much, Tristan! This interview is extremely helpful and full of practical advice.
…………………….
Let’s connect on Instagram & Twitter!